Alice Walton announces new Whole Health Institute, Chopra Medical Library
by January 15, 2020 5:45 pm 23,800 views
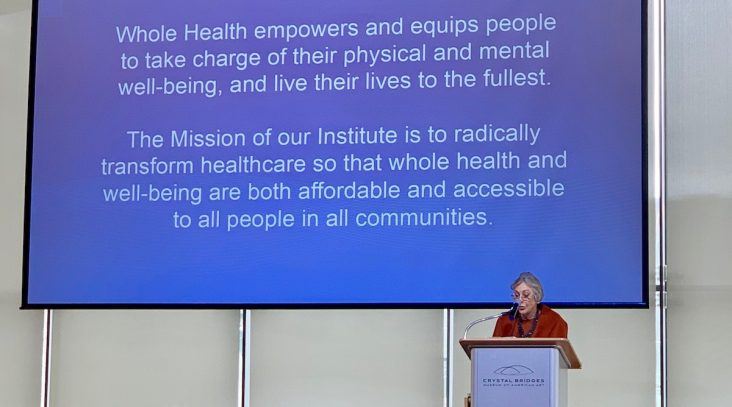
Alice Walton, philanthropist and daughter of Walmart founders Helen and Sam Walton, announces the Whole Health Institute during the Northwest Arkansas Council’s winter meeting in Bentonville.
The healthcare system is broken, and more aptly reflects a disease-care system, according to Alice Walton, philanthropist and daughter of Walmart founders Helen and Sam Walton.
She spoke Wednesday (Jan. 15) at the Northwest Arkansas Council’s winter meeting in Bentonville and announced the formation of the Whole Health Institute and Chopra Medical Library. Walton said the center will be in Bentonville and will work to improve the health in the region and around the state with impacts that will also be felt across the nation.
“We have a system that is piecemeal at best and still not affordable for many, despite its annual costs which are 17% of the nation’s GDP,” Walton said. “We need a holistic approach that incorporates mind, body and spirit. Whole health tools do exist around the country and we want to be part of the solution to change healthcare.”
Details on the new center were not fully revealed on Wednesday, and officials declined to provide cost estimates on the initial launch of the institute and estimates on annual operating costs.
Walton said she has named an executive team to lead the project. Dr. Tracy Gaudet is the executive director for the Whole Health Institute. Walton has also added a small executive team to help her get the project off the ground. That team includes Dr. Amanda Hull, director, Whole Health delivery systems and Dr. James Marzolf, director, health sector finance and policy.
Gaudet is the former executive director of the Veterans Health Administration’s National Office of Patient Centered Care and Cultural Transformation. According to the VA, the office was responsible for “a fundamental re-envisioning and redesign in the philosophy and practice of healthcare delivery for our Veterans and our Nation.” Prior to her time at the VA, Gaudet was with the Duke University Health System where she served as executive director of Duke Integrative Medicine from 2001 to 2010. Prior to her time at Duke, Gaudet was the founding executive director of the University of Arizona Program in Integrative Medicine.
BOLD IDEAS AND BRILLIANT MINDS
Walton said once the new system is created, the plan is to spread it throughout the state and region.
“One thing the [Northwest Arkansas] Council is known for is working on bold ideas and getting things done,” Walton said “This doesn’t happen through competition, but it happens through collaboration between our hospital systems, University of Arkansas for Medical Sciences, insurance companies, doctors and other healthcare providers working with brilliant minds in finance and policy to design a system that rewards health and reduces costs.”
She described the Chopra Medical Library as a center where healthcare professionals and laymen can enhance their learning from a global collection of research journals. The library is named for Deepak Chopra, a New York Times bestselling-author who Walton said has helped her throughout many years. Walton said the future will be one of more health and wellbeing, less pain and fewer chronic conditions like diabetes and obesity. It will involve more self-care creating less need for clinical and pharmaceutical treatments. The end result, Walton said, should be to reduce healthcare costs and better health outcomes.
“The U.S. is 37th in the world for life expectancy and we spend way more than other countries who have much better outcomes. We know 75% of healthcare costs are a result of chronic conditions, which more than not from patient behaviors and choices,” Walton said.
A ‘SYSTEM PROBLEM’
Gaudet said despite the U.S. spending in healthcare, the life expectancy rate is next to Cuba, at the low end of the spectrum. She said heart disease is the No. 1 killer of Americans but what most don’t know is the 1.3 million preventative angioplasty procedures done annually at a cost of $48,000 each don’t prevent future heart attacks. Behavior is a better predictor. The same is true for heart bypasses in the U.S. done as preventative measures at a total cost of $44 billion. She said these are important procedures that can save a life during a heart attack but they alone don’t prevent future cardiac arrests.
“We have a system problem that has to be unwound,” she said.
Gaudet outlined five initial priorities for the new center. At the top of the list will be to focus on healthcare delivery and partnering with healthcare systems in the region and around the state to create and demonstrate a new delivery system for whole healthcare. The center also will partner with self-insured employers to improve the health of their workforce and also reduce costs. Then the focus is to create whole health communities with NWA First being a living laboratory and model for the state and nation at large. Continued planning for the institute will be important amid collaboration between the community and the council.
The institute also will focus on finance and policy around improved healthcare for better outcomes by putting together the business case for the transformation. It will work with payors to transform to a value-based model as well as advocate for national healthcare reform. Healthcare education for practicing clinicians, medical school and existing professions and new health professions, including peers, will be another institute focus.
TAKING OWNERSHIP
Marzolf presented a business case to the group that was done with the Veteran’s Administration Health Care system over the past two years. He said looking at 204,528 veterans who received outpatient and inpatient care between fiscal 2019 and half of fiscal 2019, the total savings were $838 million after using the Whole Health Institute approach.
He said the VA has $720.853 million in cost avoidance from outpatient services, and $117 million saved from inpatient services. The cost avoidance on pharmaceuticals was $4.25 million.
Gaudet said patients in the new system will take control of their own healthcare plans. She said instead of going into the doctor’s office and waiting for their assessment from a problem list the doctor has created, the patient will tell the doctor what their aspirations are from running marathons to losing weight or just living longer to be with family. The doctor will then take that aspiration and work with the patient on overall health objectives that should include diet and stress relievers in addition to labs and drug therapy. She said when this works, patients have greater control of their health outcomes, and by taking ownership with direction from healthcare professions they have a greater shot at success.
Nelson Peacock, CEO of the Northwest Arkansas Council, told Talk Business & Politics the Whole Health Institute will be significant in the region’s mission to become a healthcare destination, a mission the council made a priority last year.
“We believe it will go a long way in helping us with medical specialties and look forward to ongoing developments,” Peacock said. “All of the local healthcare systems have signed on to work together in this initiative.”
