Northwest Arkansas medical executives, elected officials address medical residency shortage
by August 12, 2019 4:49 pm 1,216 views
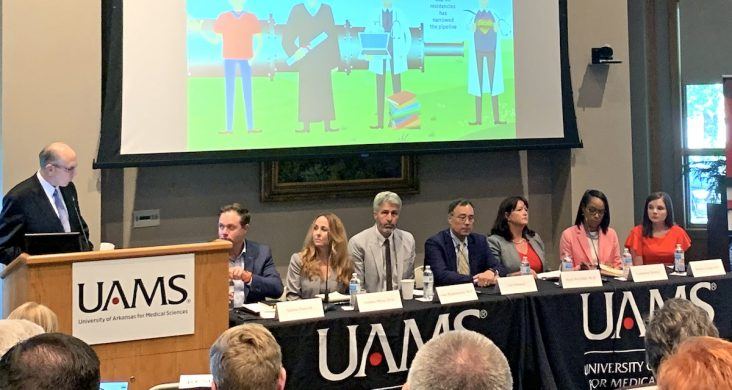
The University of Arkansas for Medical Sciences hosted a summit in Springdale on Monday to discuss the importance of expanding graduate medical education slots in the region and state. The panel moderator was Dr. Christopher Westfall, dean of UAMS College of Medicine. Panelists were (left to right) Nelson Peacock, CEO of Northwest Arkansas Council; Sen. Missy Irvin, R-Mountain View; Dr. Drake Rippelmeyer, physican at Veterans Health Care System of the Ozarks; Len Marquez, senior director of government relations AAMC; Pearl McElfish,vice chancellor for UAMS in Fayetteville; Lashannon Spencer, CEO of Community Health Centers of America; and Dr. Mikaila Calcagni, a resident physician at UAMS.
The shortage of medical residency programs is not just a problem in Northwest Arkansas, it’s a national crisis, according to healthcare workers and execs who convened Monday (Aug. 12) in Springdale to discuss challenges around funding more coveted medical residency slots.
The Association of American Medical Colleges (AAMC) predicts a national shortage of 46,900 to 121,900 physicians by 2032 which includes a shortfall of a minimum of 21,100 primary care doctors, 28,500 specialists and 14,300 surgeons.
The University of Arkansas for Medical Sciences (UAMS) hosted the panel discussion to call attention to the impact on Arkansas and discuss funding challenges. Graduate medical education, or GME, entails the three to seven years of residency training required for licensure. It comes after four years of college and a bachelor’s degree and four years of medical school.
Pearl McElfish, vice chancellor of the Northwest Arkansas campus of UAMS in Fayetteville, said in Arkansas there will be 439 medical school graduates in the next two years. There are just 290 residency slots, which means 150 doctors will have to go out of state to do their residency training.
“We are subsidizing the healthcare workforce for our neighboring states that have more residency slots. We invest in these students for eight years of higher education and then lose them to Texas or some other state because we don’t have enough residency slots,” McElfish said Monday. “When we don’t keep our doctors, that will become a health care problem in the future.”
In the past couple of years, Northwest Arkansas has increased its residency slots from 27 to 69, but the need is roughly 200 to 250 for the growing region. She said it will take multiple solutions to tackle this complex problem which is bound up by funding.
U.S. Sen. John Boozman, R-Ark., attended Monday’s panel discussion. He said he is working to expand the cap on GME funding put in place in the 1997 Balanced Budget Act. The act caps the number of residents a hospital can claim for Medicare GME. New legislation would increase resident slots by 3,000 annually between 2021 and 2025. Half of those slots would be in specialty fields. Boozman said Medicare reimbursement is also low in Arkansas and too often homegrown talent will leave the state for residency and start their practices in states like Texas which has higher Medicare reimbursement.
AAMC reports there are 38 medical residents per 100,000 in population, which is deemed a shortage of slots. In Arkansas, there are 26 residents per 100,000 people and in Northwest Arkansas, there are 12 residents per 100,000 in population.
“The number of available physicians per population in the Natural State is among the lowest in the nation and providers of all specialties are facing a serious shortfall, especially in the rural communities,” Boozman said. “The bill Senator Bob Menendez and I introduced will lift the antiquated cap on Medicare-supported doctor training slots, creating 15,000 residency training slots across the country over five years. It is a small step, but one that will go a long way to addressing this dire need in Arkansas and at the national level.”
The Northwest Arkansas Council estimates the region loses nearly $1 billion a year in economic impact because of outmigration of healthcare services, particularly specialty services. The council crafted a plan to reverse that trend with a long-range plan that begins with obtaining more residency slots in the region to handle all of the medical school graduates. That is step is the first of a three-step plan.
Nelson Peacock, CEO of the Northwest Arkansas Council, also took part in the panel discussion. He shared the importance of getting all healthcare providers in the region and state on the same page.
“Regional leaders are working collaboratively to address these challenges.. Changes in federal policy that expand GME, such as those proposed by Senator Boozman, are critical. Increasing GME will allow us to train more doctors here and give us a better chance to retain them in the long term,” Peacock said.
Len Marquez, senior director of government relations for AAMC, said funding of residency programs is a complex model as it pertains to Medicare-funded slots. He said Medicare accounts for about 30% of the AAMC baseline cost, which is about $100,000 per slot per year. He said states can also offer funding help through rebates and the rest is comprised of private funds and philanthropy. Lack of specialty care is also a big issue in the region and state. Marquez said fellowships, which are additional specialty training following residency, only get half the reimbursement costs from Medicare.
Dr. Steve Goss, CEO of Mercy Clinics in Northwest Arkansas, said the lack of fellowship slots are also a big issue and something that will have to be tackled if the region is to become a healthcare destination. He said all residency slots that exist in the region are for internal medicine. He said there would need to be some specialty residency slots come online if the region is going to be able to meet its goals and stop the out-of-state flight for specialty care.
Arkansas Sen. Missy Irvin, R-Mountain View, said during the panel discussion that the demand for physicians in rural Arkansas is dire. Her husband set up practice in Mountain View 23 years ago because the couple wanted to raise their family in a small town. She said physician training is a workforce issue and deserves equal funding.
“It’s great that we have workforce funding for welders and cosmetology. Those are important jobs. But no more so than a doctor who works in rural communities. A doctor’s private practice in a rural community will add economic value supporting pharmacies, paying taxes and creating jobs. We have got to start thinking about physician’s training as a workforce issue,” Irvin said.
Susan Barrett, a former Mercy executive, closed the event by challenging all the medical care executives, advocates and elected officials to use all the power they each wield to push for more residency slots to benefit the entire state.
“At this moment in time, we are not inspired to be compared to the bottom of anything whether that’s Medicare reimbursement or attracting and retaining residents or being unhealthy people. … We are proud, pleased and grateful. … We will retain our brightest and best and send them to world-class facilities. This is a mighty charge. We can do this … it will take all of us to do this,” Barrett said.
