Gov. Hutchinson touts health care bills in press conference
by March 25, 2016 11:19 am 200 views
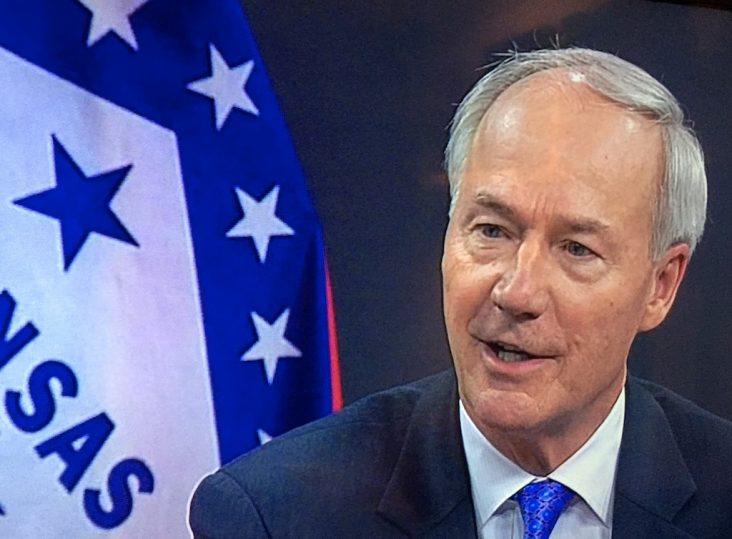
Gov. Asa Hutchinson touted his legislation in the upcoming health care special session as “historic” and “unique” during a press conference Friday at the Capitol.
Legislators will gather April 6 to consider Hutchinson’s Arkansas Works program, which is his replacement for the private option. The private option uses federal Medicaid dollars to purchase private insurance for adults with incomes up to 138% of the federal poverty level. Created in 2013, it now covers more than 200,000 Arkansans, but it has been controversial since it was created and by law ends at the end of this year.
Arkansas Works differs from the private option in its emphasis on job training for recipients, its requirement that recipients pay up to 2% of their income in premiums, and its requirement that beneficiaries enroll in employer plans when qualified plans are available to them.
The bill includes incentives for employers to offer health insurance. Hutchinson said it intentionally is flexible on what those incentives would be so they can be negotiated. The incentives at first would focus on small employers but also could be used for larger ones “down the road.”
Hutchinson also is supporting a second bill, the Arkansas Medicaid Reform Act of 2016, that would create a managed care system in Medicaid for individuals with developmental disabilities, those receiving behavioral health services, and all dental services.
In that model, a private company or companies would manage parts of the Medicaid program under contract with the Department of Human Services, receiving a set amount per member. The vendor would make higher profits for cost-efficient care while bearing the financial burden if it fails to meet targets.
Using numbers provided by The Stephen Group, a consultant for legislators on the Health Reform Legislative Task Force, Hutchinson said the managed care model would create $1.4 billion in estimated overall Medicaid savings from fiscal year 2017 to fiscal year 2021. The bill includes a bill of rights for medical providers that, among other provisions, requires that they be paid no less than the prevailing Medicaid fee schedule unless a different rate is negotiated by the provider and the managed care organization. It also is meant to protect beneficiaries through measures such as a requirement that no limit be placed on medically necessary visits to a primary care provider.
Hutchinson said the bill empowers the Legislature over the executive branch and would place restrictions on managed care organizations.
It also creates a trust fund meant to reduce the waiting list of 3,000 individuals with developmental disabilities awaiting state services that enable them to stay in their homes and communities.
A competing bill supported by some legislators, the Managed Fee-For-Service Act of 2016, would create a different type of cost-saving system. A vendor would provide administrative services including an independent assessment, plan of care, quality assurance, and outcomes measurement. The Department of Human Services would create a methodology for incentive payments for a contractor that meets benchmarks. If the vendor provides lesser care or fails to meet contracted benchmark savings, it would pay an administrative fee.
Supporters of that bill say it would involve less risk than managed care. Hutchinson said that model actually would be riskier because it’s a new concept, while managed care has been tried in many states.
The bills require only a majority vote to pass during the special session. Funding mechanisms, however, require a three-fourths vote in the fiscal session that will follow beginning April 13. Hutchinson didn’t speculate on where the vote count currently lies. However, he said he was not seeking a three-fourths majority during the special session.
“Each session has a different dynamic. … My goal is to get it passed in the authorizing or the special session by majority vote, and then to be able to succeed in the appropriation session, through the budget, but (there is a) totally different analysis, and the number count will be totally different,” he said.
Other issues circulating among policymakers include an alternate way of selecting appellate judges other than elections, and two ethics bills that are being circulated by Democratic legislators. One of those bills would require more disclosure of campaign contributions as a way of combatting so-called “dark money.” The other would give citizens who are victims of judicial misconduct an avenue for filing suit against the official.
Hutchinson said he would oppose discussing those issues until a second special session focusing on highways, which is tentatively scheduled to occur after the fiscal session. Hutchinson said policymakers should “stick to our knitting.”
Hutchinson’s office this week sent a memo to lawmakers saying that a pilot program drug-testing Temporary Assistance for Needy Families recipients instead will be in effect statewide. Hutchinson said the legislation was supported by a strong majority of Republicans and Democrats and that it faced legal challenges if done in isolated areas. He said the objective is not to reduce the number of welfare beneficiaries but to reduce drug dependency.
